
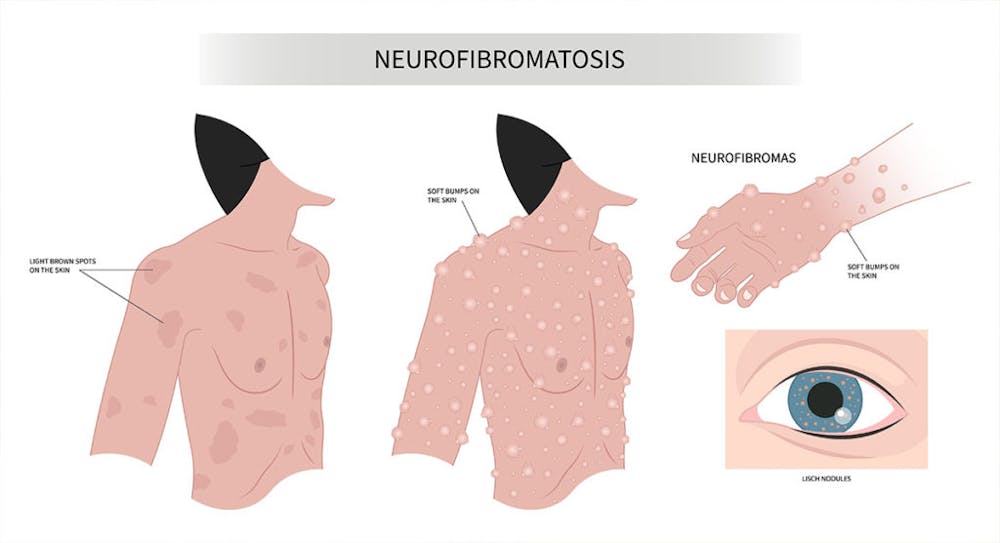
People with neurofibromatosis have a mutated gene that causes tumors to grow on the nerves of their bodies. While these tumors can be benign, they can also cause serious complications if left untreated. Neurofibroma removal treatment is an important step in managing this condition and reducing the risk of further complications. Depending on the type of neurofibromatosis and the size and location of the tumor, removal may involve surgery or other treatments such as radiation therapy or chemotherapy. Despite its potential benefits, there are still some risks of neurofibromatosis removal treatment.
Common complications associated with neurofibromatosis removal treatment include pain, infection, bleeding, nerve damage, and scarring. In addition to physical side effects, patients may also experience psychological issues such as anxiety or depression. It is important for patients to discuss any concerns they have with their doctor before undergoing any type of neurofibromatosis removal treatment so that they are aware of all potential complications. With proper care and monitoring, most people who undergo neurofibromatosis removal treatment experience positive outcomes and improved quality of life.
Possible Complications Associated with Neurofibroma Removal
1. Infection
Infections can occur after any type of tumor removal surgery, including those used to treat different types of neurofibromatosis. Bacteria entering the wound during or after surgery can cause infections and can lead to serious complications if not treated promptly.
Patients should take extra care to keep their wounds clean and dry and follow their doctor’s instructions for post-operative care. If an infection does occur, it is important to seek medical attention right away in order to reduce the risk of further complications from neurofibromatosis treatment.
2. Changed sensations
Neurofibromatosis removal treatment can also cause changes in sensation in the area of the tumor. This can include numbness, tingling, or burning sensations that may persist for some time after the procedure. In some cases, these sensations may be permanent and require additional treatments to manage. Neurofibromatosis patients should discuss any changes in sensation with their doctor so that they can receive appropriate care and treatment if necessary.
3. Scarring
Scar tissue forms when the body repairs itself after surgery, and this can be especially pronounced in patients with neurofibromas due to their increased risk for scarring.
Depending on the size of the tumor and the type of surgical treatment used, patients may experience aberrant or hypertrophic scarring. Aberrant scarring occurs when the wound heals abnormally, resulting in an uneven or raised scar. Hypertrophic scarring produces thick and raised scars that may be painful or itchy.
4. Hemorrhage
Hemorrhages can occur when the surgical procedure involves cutting through thickened skin or removing a tumor of significant size. Patients with a history of bleeding disorders like blood pressure or those taking anticoagulants are at an increased risk for hemorrhage during neurofibromatosis removal treatment. Symptoms of hemorrhage include excessive bleeding, bruising, and swelling in the area of the surgery. If any of these symptoms occur, it is important to seek medical attention right away in order to reduce the risk of further complications from Neurofibromatosis treatment.
In order to reduce the risk of hemorrhage during neurofibromatosis type 1 removal treatment, patients should discuss their medical history and any medications they are taking with their doctor before undergoing neurofibromatosis surgery. Additionally, patients should follow all pre-operative instructions carefully and take extra care to keep their wounds clean and dry after surgery in order to reduce the risk of infection.
5. Nerve damage
Nerve damage is a potential complication of neurofibromatosis removal treatment. This can occur when the tumor is located near or on peripheral nerves, such as those that control movement and sensation in the arms and legs. It can also occur when tumors are located near or on the optic nerve (optic glioma), which controls vision. In some cases, nerve tissue may be damaged during surgery due to the size of the tumor or its location.
Peripheral nerve sheath tumors are benign tumors that can cause nerve damage if they are not removed properly. Acoustic neuromas, which are benign tumors that grow on the hearing and balance nerves, can also cause nerve damage if they are not removed correctly. The risk of nerve damage increases with larger tumor sizes and more complex surgical procedures.
6. Neuroma formation
Neuromas are small, benign tumors that can form in the area of the surgery site. They are most commonly seen in patients with cutaneous manifestations of neurofibromatosis, such as cutaneous neurofibromas. Neuromas can also occur in patients who have had surgery to remove larger tumors or those with more complex tumor types.
Neuroma formation is one of the most common side effects associated with neurofibromatosis removal treatment. Patients may experience pain, numbness, tingling, or burning sensations at the site of the neuroma. In some cases, these symptoms may be permanent and require additional medical intervention to manage them. Patients should discuss any concerns about neuroma formation with their doctor before undergoing surgery so that they are aware of all potential risks involved.
7. Chronic pain & Numbness/tingling sensations
Patients may experience these symptoms due to the presence of painful neurofibromas in patients with cutaneous neurofibromatosis. Or due to nerve damage caused by the surgery itself. Symptoms of severe pain can include aching, burning, stabbing, or throbbing sensations that last for weeks or months after the surgery.
Numbness and tingling sensations can also occur as a result of nerve damage caused by plastic surgery. It is important for patients to seek medical attention from pain management specialists if they experience any of these symptoms following their surgery. Pain management specialists can provide treatments such as over-the-counter pain relievers, physical therapy, and lifestyle modifications to help reduce pain and improve quality of life.
8. Not all tumors are removable
Not all tumors are removable, and this can present difficult issues for those undergoing neurofibroma-removal surgery. In some cases, cancerous tumors may be too large or too close to delicate nerve tissues which complicates their removal. In these cases, additional surgery may be necessary to remove the tumor without damaging the surrounding tissue.
Facial nerve damage is a potential complication of neurofibroma-removal surgery, as it is a delicate nerve that can easily be damaged during the procedure. It is important for patients to discuss any concerns they have with their provider about the risks associated with their particular type of surgery before proceeding.
The Impact of Stress and Anxiety on Recovery from Neurofibroma Removal Treatment
The impact of stress and anxiety on recovery from this hereditary disorder is significant. Patients with this condition often experience emotional distress due to limited daily activities. Surgery side effects, such as pain, numbness, tingling, or burning sensations can also cause additional stress and anxiety. Furthermore, candidates for surgery may be concerned about the potential risks and side effects of surgery.
Since family history is an important factor for neurofibromatosis, genetic testing can help identify those who are at risk for developing neurofibromatosis and provide insight into the best course of action for treatment. Unfortunately, there is no cure for neurofibromatosis and many medical issues can arise from nearby tissues that are in contact with tumors or other growths.
Stress and anxiety can have a negative effect on recovery from neurofibromatosis treatment. It is important for patients to follow their after-care instructions and discuss any concerns they have with their doctor before undergoing surgery so that they are aware of all potential risks. Additionally, it is beneficial to seek out support from family members or friends during this time in order to reduce feelings of isolation or fear associated with the procedure.
What to do if you have a diagnosis of Neurofibromatosis?
The first step is a referral to a Neurofibromatosis Clinic or a neurologist or geneticist with expertise. After a thorough workup, there may be a requirement to see a neurosurgeon if there is a need for brain tumor surgery or an orthopedic surgeon for issues in the spinal cord.
Frequently, a plastic surgeon with a specialization in neurofibromatosis addresses tumors that are causing symptoms such as pain or disfigurement. Dr. Panossian has treated neurofibromatosis Pasadena patients for over a decade and recognizes the unique requirements of this patient population. Our healthcare team can assist you with the proper referral. Schedule a consultation today.


