This innovative treatment is designed to address various concerns related to facial symmetry, contouring, and harmony, providing you with a rejuvenated and balanced appearance.
Gracilis Muscle Transplant (Masseter Nerve): A Comprehensive Overview
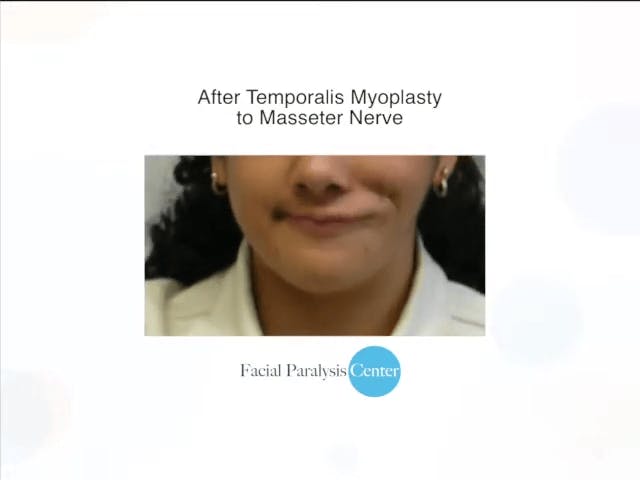
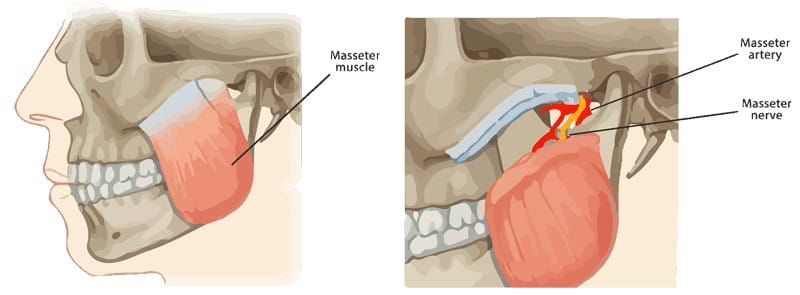
In other words, there are several other muscles that accomplish the same goal; therefore, sacrificing the muscle results in no loss of function in the thigh. Only a small, thin segment of the gracilis muscle is taken from the thigh along with its blood and nerve supply. The muscle is then moved to the paralyzed side of the face where it is connected to local nerves and blood vessels. In this case, it is attached to the masseter nerve on the same side as the paralyzed face. After 3-6 months, the muscle becomes active and contracts to move the corner of the lip. The masseter nerve is derived from a branch of the fifth cranial nerve (trigeminal nerve) and is responsible for activating the bite via the masseter muscle. The reason that it is used in facial reanimation surgery is because biting is an analogous function to smiling. In other words, to a certain degree human beings trigger their biting muscles when smiling.
There are several advantages to using the masseter nerve to power the gracilis muscle over a cross-face nerve graft. First, only a single surgery is required to achieve lip movement as opposed to two. Second, recent studies suggest that gracilis muscles connected to the masseter nerve deliver a greater contractile force over a cross-face nerve graft, making the corner of the mouth rise more aggressively. Third, the time to smile reanimation is significantly abbreviated (3-6 months vs 12-18 months). The main disadvantage to using the masseter nerve is that activation of the smile is not spontaneous, since stimulation is derived from the fifth cranial nerve used in biting. In other words, initially, a person would need to trigger a bite to create a smile. Physical therapy is required to re-train the gracilis muscle for smiling. However, this is achievable in the great majority of patients.