This advanced surgical technique is designed to restore facial movement and expression in individuals affected by facial paralysis or weakness.
Gracilis Muscle Transplant (Cross Face Nerve Graft) A Detailed Procedure Overview
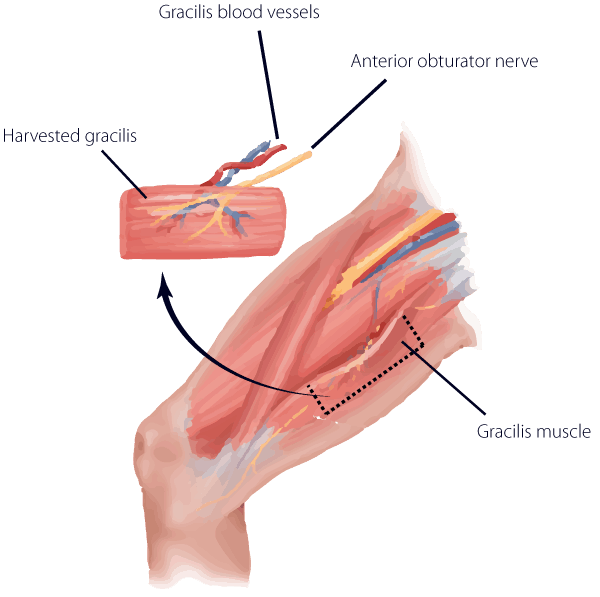
During this initial surgery, a long nerve is harvested from the lower leg (sural nerve). This nerve supplies only a small patch of sensation to the outer part of the foot, and therefore, results in no noticeable loss of function. It is typically harvested from the leg with three small incisions and does not result in disfigurement. The nerve is then implanted into the unparalyzed side of the face to one of the working branches of the facial nerve responsible for generating an ideal smile. It is then tunneled within the face and banked in the upper lip, close to the paralyzed side of the face. After a period of 6-12 months, nerve regeneration reaches the terminal point of the nerve graft and is ready for powering the gracilis muscle. The gracilis is a long muscle located in the inner thigh. It is responsible for moving the hip inwards (or, adduction). It is a redundant muscle for this function. In other words, there are several other muscles that accomplish the same goal, therefore, sacrificing the muscle results in no loss of function in the thigh. Only a small, thin segment of the gracilis muscle is taken from the thigh along with its blood and nerve supply. The muscle is then moved to the paralyzed side of the face where it is connected to local nerves and blood vessels. In this case, it is attached to the cross-face nerve graft. After a period of 6-12 months, the muscle becomes active and contracts to move the corner of the lip. The primary advantage of using a cross-face nerve graft to power the gracilis muscle is the spontaneous nature of the smile following reanimation. In other words, the neural pathways for initiating a smile occur through normal channels via the facial nerve. Therefore, there is no re-training of muscles required as there would be with temporalis muscle transfers or gracilis muscles connected to the masseter nerve (fifth cranial nerve used for biting).