Pediatric facial paralysis is a condition that affects a child's ability to move the muscles of their face, leading to difficulties with expression, eating, and speaking.
Facial Paralysis In Kids


Addressing Pediatric Facial Paralysis
One of the core focuses of Dr. Panossian’s practice is the treatment of facial paralysis in children. He has performed hundreds of surgeries to reconstruct patients with facial paralysis. Based on his extensive experience in the field, Dr. Panossian created the Facial Paralysis Center at Children’s Hospital Los Angeles, bringing together multiple specialists to treat patients affected by facial paralysis.
Trained at Harvard and at the Hospital for Sick Children in Toronto with Dr. Ron Zuker, he is an expert in both Zuker and Labbé smile surgery techniques. In addition to performing the gracilis muscle transfer and cross-face nerve graft, Dr. Panossian has modified and refined the temporalis myoplasty (Labbé technique) to get consistent results and shorter recovery times.
For most patients, this is now an outpatient procedure. Other necessary procedures for correction of eyelid drooping, brow asymmetry, and lower lip balancing are now offered simultaneously. Dr. Panossian’s modifications have improved the time to reanimation and overall patient satisfaction. In addition, his specialty in the complex world of pediatric plastic surgery gives him an edge in addressing facial paralysis in adults as well. More information is available in the Facial Paralysis section of this website.
The face can be broken into 3 key areas of facial nerve function and expression. The upper third deals with forehead elevation. The middle third focuses on eyelid closure. And the primary function of the lower third function is dynamic smile and mouth movement.
Facial Paralysis Conditions in Kids

Forehead Elevation
With paralysis of the forehead, the ability to raise the brow or create wrinkles is affected. People with forehead paralysis are not necessarily noticed right away. However, with animation and simple gestures, the lack of movement becomes obvious. Sometimes, forehead paralysis may result in gradual drooping over the upper eyelid. This can worsen over time and can even partially block vision.
As with other areas of the face, options are available for treatment of forehead paralysis. Although a paralyzed forehead may mimic a “permanent Botox®” effect, many people don’t care for the look, especially when only one half of the forehead is affected. For those wishing to have a more uniform appearance, Botox® injections to the unaffected side may produce the desired appearance. However, these injections may be required every 3 to 6 months to maintain the effect. Another option may be to permanently paralyze the normal side of the forehead with a surgical procedure. For patients experiencing problems with their vision due to a heavy, droopy forehead, a browlift will restore the height of the brow to a desirable level. Dr. Panossian has studied and refined these techniques over many years. Arrange a consultation today to discuss your options.

Child with facial paralysis trying to raise forehead.
Eye Closure
Paralysis of the eyes and eyelids can result in a number of problems. The most serious problem is the inability to close the eye, which can remain open while sleeping. Persistent problems with eye closure may lead to drying of the cornea. In turn, this may result in permanent scarring and eventual blindness. This is the most compelling reason to treat facial paralysis.

Child with facial paralysis trying to close eyes.
Other problems include the appearance of the droopy lower eyelid. Initially, the droop may be subtle, but with time, the lower eyelid will fall further. This causes a noticeable deformity and one of the stigmata of facial paralysis. The upper eyelid may also have trouble doing its part to close the eye and can worsen the problem of the “wide eyed” look. Lastly, the dynamic effect of blinking can be affected. This is typically one of the most difficult functions to restore.
Several solutions exist for the variety of problems that can affect the eye in facial paralysis. The decision to pursue surgery is made in conjunction with an ophthalmologist’s evaluation. If signs of corneal scarring (ie, keratopathy) are present despite aggressive lubrication regimens, then the decision to undergo surgery is made urgently. Alternatively, if eyelid drooping (ie, lagophthalmos) is causing a severe cosmetic deformity, then one can also proceed with surgical correction.
A number of surgical techniques are available to correct eyelid paralysis depending upon severity. These include placement of an upper eyelid weight, lower eyelid tendon sling, or tarsorrhaphy (suturing outer part of upper and lower eyelids together), among others.
Synkinesis is the involuntary movement of facial muscles that can occur after recovery of the facial nerve. This happens most often in the setting of Bell’s palsy and can be quite disconcerting for patients. It is the result of miswiring of the downstream branches of the facial nerve during the process of nerve regeneration. In the setting of facial paralysis, eyelid twitching may be triggered by voluntary activation of other facial muscles, such as smiling or moving the mouth. Treatment to correct this problem can include surgical denervation of the interconnections between the involved muscles or with use of Botox®.
Whether mild or severe, correction of eyelid problems is an important part of any treatment plan for facial paralysis. Dr. Panossian’s years of experience and specialized training in the correction of facial paralysis have assisted hundreds of patients seeking relief from their symptoms.
Inability to Smile
Your smile is one of the most unique characteristics about your face. Losing the ability to smile can have profound effects on the ability to socially interact with others, communicate, and develop one’s self image.
Numerous options are available for patients requiring reconstruction. Generally, these options could be categorized as “static” or “dynamic” in nature. Static reconstructions involve resuspending the corner of the mouth in a natural position to counteract the droop of the paralyzed face.
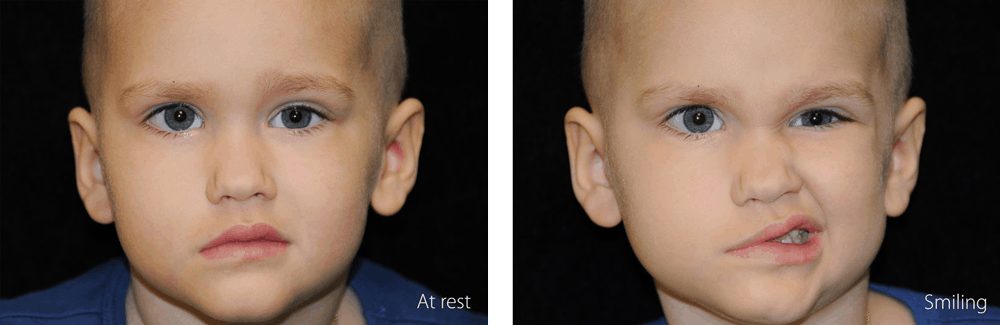
Child with facial paralysis at rest and trying to smile.
This can be done in a number of ways using several natural and artificial options. Dynamic reconstructions involve the use of techniques to re-establish muscle control of the paralyzed face. This typically involves the transfer of a muscle from another part of the body to the face where it is reconnected to a new blood supply and plugged into a functioning nerve. Over time, the new muscle gains the ability to move and re-activate the lost smile.
Numerous options are available for patients requiring reconstruction. Generally, these options could be categorized as “static” or “dynamic” in nature. Static reconstructions involve resuspending the corner of the mouth in a natural position to counteract the droop of the paralyzed face. This can be done in a number of ways using several natural and artificial options. Dynamic reconstructions involve the use of techniques to re-establish muscle control of the paralyzed face. This typically involves the transfer of a muscle from another part of the body to the face where it is reconnected to a new blood supply and plugged into a functioning nerve. Over time, the new muscle gains the ability to move and re-activate the lost smile.
Dr. Panossian has developed a new take on an old technique (ie, the Labbé technique) designed to reanimate the smile using a muscle for biting. This muscle, called the temporalis, is one of four muscles used in biting, and it is located on the side of the head. When biting, the muscle can be felt to tense up. What makes this surgery ideal is that it utilizes a nearby muscle that is already functioning to achieve a smile. Specifically, the insertion of the muscle on the lower jaw is changed so that the muscle begins to pull on the corner of the mouth. The muscle is functional for smiling from as early as several days after surgery. Over time, the muscle begins to move spontaneously when trying to smile, even though it was originally used for biting. There are numerous advantages of this technique: it can be done in an outpatient setting for most patients, scars are minimal, bulk in the cheek is significantly minimized, and time to achieving results is improved. You can read more about Dr. Panossian’s technique here.
Other methods are also available to dynamically reconstruct, not only the smile, but possibly all of the paralyzed facial muscles. In those patients presenting early on in their facial paralysis (within the first 9 to 12 months), nerve transfers and nerve grafting may be options for treatment. This entails “re-wiring” the affected facial nerve so that it receives innervation from another nerve in the face. This may be achieved via a nerve graft from the opposite (unaffected) side of the face using a branch of the functioning facial nerve. Or, a different unaffected nerve on the same side of the face may be transferred and plugged in. This first type of surgery is called a “cross-face nerve graft,” whereas the second type is a “nerve transfer.” The nerve graft is obtained from the leg through small incisions and does not result in any functional loss in the leg. The nerve transfer will utilize one of the branches of the fifth cranial nerve used for biting in most cases. Once again, there is usually no functional deficit where the nerve originated.
"Met with Dr. Panossian at an educational conference to discuss my son’s facial paralysis. Very knowledgable with a great bedside manner."
- T.W.

Additional Treatment Methods
Both static and dynamic reconstructions are complex and have pros and cons as with all surgical options. Making the decision to pursue one line of treatment over another is difficult. It involves the desires of the patient, the degree of facial paralysis present, and the patient’s own physiology. Dr Panossian is one of only a handful of experts in the world with training and skill in restoring paralyzed faces with the full complement of options, especially with the intricate task of repairing one’s smile. Call Dr. Panossian today to discuss your options.
Dr. Panossian is Founder of the Facial Paralysis Center at Children’s Hospital Los Angeles and has taken his multidisciplinary approach to his private practice. He performs comprehensive analysis and treatment of children and adults with facial paralysis.
Why Choose Dr. Panossian?
- He received his medical education at Tufts University School of Medicine.
- Graduated at the top of his class at UCLA, receiving Phi Beta Kappa and Summa Cum Laude honors.
- Was accepted into an elite combined general surgery and plastic surgery residency at the Keck School of Medicine of USC.
- Completed subspecialty training in craniofacial surgery at the Hospital for Sick Children in Toronto and Harvard Medical School.
- Was mentored by Dr. Ron Zuker in the practice of facial paralysis reconstruction. This prestigious fellowship position was available to only one surgeon in the United States.
- Is a member of the American Society of Plastic Surgeons and the highly selective American Association of Plastic Surgeons, reserved for only a select group of individuals nationally who have demonstrated excellence in academic plastic surgery.
- Is affiliated with various charitable and educational organizations, including Operation Smile and Mending Kids.
- Holds memberships in several other professional societies including the American College of Surgeons and the American Society of Reconstructive Microsurgery.
- He serves on the Board of Directors for Mending Kids and the Gondobay Manga Foundation, a non-profit organization dedicated to the improvement of lives in Sierra Leone.
- Has been nominated by his peers annually since 2012 as a “Super Doctor.”
- Served as an expert medical consultant and appeared on The Doctors, Grey’s Anatomy, and Nip/Tuck.
- Has been featured as “Top Doctor” in US News and World Report, Pasadena Magazine, and Los Angeles Magazine.






