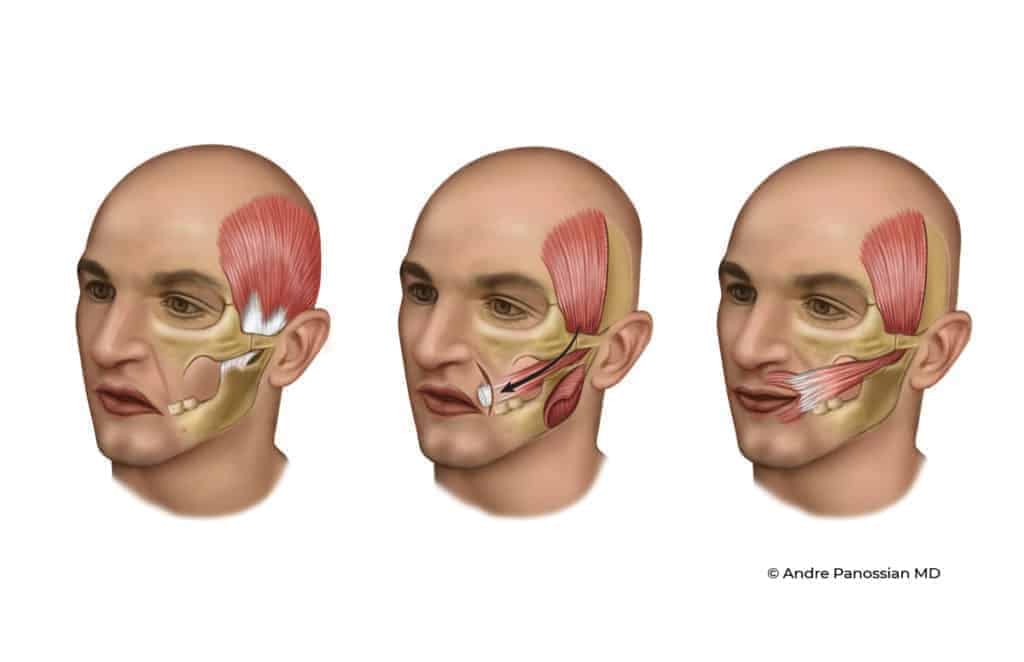
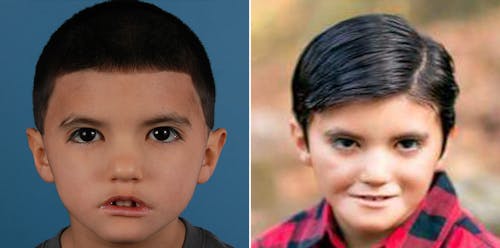
Unlock the power of your smile with smile reanimation (temporalis myoplasty), a groundbreaking procedure that restores facial symmetry and movement with natural-looking results.
Additional Smile Reanimation Treatment Options
In addition to temporalis myoplasty, several other treatment options are available for smile reanimation, each tailored to address specific cases of facial paralysis. While each treatment option has its benefits and considerations, the choice depends on factors such as the underlying cause of facial paralysis, the extent of nerve damage, and the patient's individual needs and goals. Consulting with Dr. Panossian is essential to determine the most suitable treatment plan for achieving optimal smile reanimation results.
- Gracilis Muscle Transplant (Cross Face Nerve Graft): This technique involves transplanting the gracilis muscle from the thigh to the face and connecting it to the opposite healthy facial nerve using a nerve graft. It allows for restoring facial movement by utilizing the healthy nerve supply from the unaffected side of the face.
- Gracilis Muscle Transplant (Masseter Nerve): Similar to the cross-face nerve graft, this procedure utilizes the gracilis muscle from the thigh. However, instead of connecting it to the opposite healthy facial nerve, it is linked to the masseter nerve on the affected side of the face. This approach aims to achieve smile reanimation by utilizing a nearby nerve source.
- Cross-Face Nerve Graft: In cases where the facial nerve on one side of the face is damaged or non-functional, a cross-face nerve graft involves harvesting a nerve from the healthy side of the face and grafting it onto the paralyzed side. This approach allows for the restoration of nerve function and enables facial movement.
- Nerve Transfers: Nerve transfers redirect a healthy nerve from a less critical muscle to the paralyzed facial muscles, restoring function. This approach can offer significant improvements in smile symmetry and movement.